What Is Adverse Drug Reaction: Medicines are meant to cure, prevent, or manage diseases. But what happens when they cause unintended and harmful effects? That’s where adverse drug reactions (ADRs) come into play.
According to the World Health Organization (WHO), an adverse drug reaction is defined as “a response to a drug that is noxious and unintended and occurs at doses normally used in humans for prophylaxis, diagnosis, or therapy of disease, or for the modification of physiological function.”
In simpler terms, an ADR is a harmful reaction that happens after taking a prescribed drug at the correct dose. This can range from mild discomfort to severe health complications, sometimes even leading to hospitalization or death.
In this blog, we will explore:
- What is adverse drug reaction?
- Causes of adverse drug reactions
- Types of adverse drug reactions with examples
- Difference between adverse event and adverse drug reaction
- How to report an adverse drug reaction?
- Adverse drug reaction classification
- Who can report adverse drug reactions?
Read on to know more all about adverse drug reactions in this blog!
What Is Adverse Drug Reaction?
A drug reaction becomes adverse when it causes unwanted effects, even when taken at the prescribed dose. These reactions can range from mild rashes to life-threatening conditions like anaphylaxis.
ADRs are different from side effects. While side effects are predictable and often mild (such as drowsiness from an antihistamine), ADRs are unexpected and harmful.
Examples of adverse drug reactions:
- Penicillin allergy – Severe allergic reactions like anaphylaxis.
- Liver damage from paracetamol – High doses may cause liver toxicity.
- Bleeding due to blood thinners (like warfarin) – Increased risk of internal bleeding.
According to an Indian Journal of Pharmacology study, around 6-10% of hospital admissions in India are due to ADRs.
Continue reading to know more about what is adverse drug reaction.
Causes of Adverse Drug Reactions
Adverse Drug Reactions (ADRs) can occur due to a variety of factors, including pharmacological properties of the drug, individual patient characteristics, and external influences such as medication errors or environmental exposure.
Below are the major causes of ADRs explained in detail:
1. Pharmacological Causes (Drug-Related Factors)
Many ADRs result from the way a drug interacts with the body. Some reactions are predictable and depend on the drug’s dose, interactions with other drugs or food, and the formulation of the medication.
- Dose-Related Reactions (Type A – Augmented Reactions): One of the most common causes of ADRs is excessive drug dosage, leading to toxicity. For example, an overdose of insulin can cause hypoglycemia, while excessive use of warfarin can lead to severe bleeding. Similarly, aminoglycoside antibiotics may cause kidney damage when administered at high doses.
- Drug-Drug Interactions: When two or more drugs are taken together, they may interact, either enhancing or diminishing each other’s effects. For instance, combining warfarin and aspirin significantly increases the risk of bleeding. Similarly, rifampin can reduce the effectiveness of oral contraceptives, while taking ACE inhibitors with NSAIDs may result in kidney failure.
- Drug-Food Interactions: Certain foods can affect how a drug is absorbed or metabolized. For example, grapefruit juice increases the toxicity of statins by slowing their breakdown in the liver. Vitamin K-rich foods can reduce the anticoagulant effect of warfarin, making it less effective. In another example, foods high in tyramine, such as aged cheese and red wine, can cause dangerously high blood pressure when consumed with MAO inhibitors.
- Drug Formulation Issues: Differences in drug formulation can also lead to ADRs. Some modified-release formulations may result in unexpected side effects if crushed or taken improperly. Additionally, some generic medications may have variability in bioavailability, leading to fluctuations in drug levels and effects.
2. Patient-Related Causes
Not all patients react to drugs in the same way. Factors such as genetics, age, organ function, immune response, and lifestyle choices can influence drug effects.
- Genetic Variations (Pharmacogenetics): Genetic differences can impact how an individual metabolizes a drug, leading to unexpected reactions. For example, people with G6PD deficiency who take primaquine may experience severe hemolysis (red blood cell breakdown). Similarly, individuals with HLA-B*5701 who take abacavir are at high risk of a life-threatening allergic reaction. Poor metabolizers of CYP2C19, a liver enzyme, may find that clopidogrel (a blood thinner) is less effective, increasing the risk of blood clots.
- Age-Related Factors: Both newborns and elderly patients are at higher risk of ADRs due to differences in metabolism and organ function. Neonates cannot effectively break down certain drugs, leading to toxicity, such as in Gray baby syndrome, caused by chloramphenicol accumulation. Similarly, elderly patients are more sensitive to benzodiazepines, increasing the risk of drowsiness and falls.
- Organ Dysfunction (Liver, Kidney, Heart): Patients with impaired organ function often experience altered drug metabolism and elimination, leading to toxicity. For example, in liver failure, drugs like paracetamol can accumulate and cause liver toxicity. Similarly, in kidney disease, drugs such as digoxin can build up in the body, leading to severe side effects. In patients with heart failure, beta-blockers may not be properly metabolized, leading to excessive drug accumulation.
- Immune System Hypersensitivity (Allergic Reactions): Some patients experience allergic reactions due to an overactive immune response to certain drugs. For example, penicillin can cause anaphylaxis, a life-threatening allergic reaction. Similarly, NSAIDs can trigger angioedema, a condition where severe swelling occurs in the skin and airways, leading to breathing difficulties.
- Pregnancy & Lactation: Pregnant and breastfeeding women need to be cautious, as certain drugs can harm the fetus or be excreted in breast milk. For example, isotretinoin (used for acne) is known to cause serious birth defects if taken during pregnancy. Similarly, tetracycline antibiotics can permanently stain the teeth of developing babies when used by pregnant or breastfeeding mothers.
- Lifestyle Factors (Smoking, Alcohol, Diet): Certain lifestyle choices can alter drug metabolism. Smoking speeds up the breakdown of theophylline, making the drug less effective for asthma treatment. Meanwhile, alcohol consumption while taking metronidazole can cause severe nausea and vomiting due to a disulfiram-like reaction.
To know more about ADRs from LLRI Expert Madhura Adhikary, watch the video where she will thoroughly explain “what is adverse drug reaction” to you!
3. External Factors
Some ADRs occur due to external factors, including human errors in prescribing, dispensing, or administering medications, as well as environmental influences.
- Medication Errors (Human Mistakes): Errors in drug prescription, dosing, or administration can result in ADRs. For instance, administering insulin instead of heparin can cause severe hypoglycemia. Similarly, giving a drug by the wrong route (e.g., IV instead of intramuscular) can lead to serious complications.
- Environmental & Occupational Exposure: Environmental factors can influence how the body reacts to certain drugs. Exposure to pesticides or heavy metals may enhance the neurotoxic effects of some medications. People working in industries with high chemical exposure may experience increased drug toxicity due to enzyme interactions.
Types of Adverse Drug Reactions with Examples
These adverse drug reaction classifications help in understanding ADRs and managing them effectively. Dose adjustment, genetic screening, alternative drugs, and patient counseling are essential strategies to prevent serious adverse effects. Now that you are aware of what is adverse drug reaction, let’s explore the types of ADRs.
1. Dose-related (Augmented) ADRs
These are predictable and occur due to excessive pharmacological effects of the drug.
Examples:
- Insulin: Hypoglycaemia
- Warfarin: Bleeding
- Amlodipine (Calcium channel blocker): Swelling in the legs (pedal edema)
- Opioids (Morphine, Codeine): Respiratory depression
- Beta-blockers (Propranolol, Atenolol): Bradycardia (slow heart rate)
2. Non-dose-related (Bizarre) ADRs
Unpredictable, often immune-mediated or genetic.
Examples:
- Penicillin: Anaphylaxis
- Chloramphenicol: Aplastic anemia
- Carbamazepine: Stevens-Johnson Syndrome (SJS) in HLA-B*1502 carriers
- Halothane (anesthetic): Hepatitis
- Sulfonamides: Drug-induced hypersensitivity reactions
3. Dose-related and Time-related (Chronic) ADRs
Occurs with long-term drug use, leading to cumulative toxicity.
Examples:
- Corticosteroids (Prednisolone, Dexamethasone): Osteoporosis, adrenal suppression
- Methotrexate: Liver fibrosis with prolonged use
- Bisphosphonates (Alendronate, Risedronate): Osteonecrosis of the jaw
- NSAIDs (Ibuprofen, Diclofenac): Chronic kidney disease
- Amiodarone: Thyroid dysfunction (hypothyroidism or hyperthyroidism)
4. Time-related (Delayed) ADRs
Appears after a long delay, even after stopping the drug.
Examples:
- Isotretinoin (for acne): Birth defects (teratogenic)
- Chemotherapy drugs (Cyclophosphamide, Cisplatin, Doxorubicin): Secondary cancers like leukemia
- Diethylstilbestrol (DES, old estrogen therapy): Vaginal cancer in daughters of exposed mothers
- Fluoroquinolones (Ciprofloxacin, Levofloxacin) Tendon rupture, occurring weeks or months later
- Radiation therapy or alkylating agents: Increased risk of secondary malignancies
5. Withdrawal (End of use) ADRs
Occurs when a drug is suddenly discontinued after long-term use.
Examples:
- Beta-blockers (Propranolol, Atenolol): Rebound hypertension
- Benzodiazepines (Alprazolam, Diazepam, Lorazepam): Withdrawal seizures, anxiety
- Opioids (Morphine, Heroin, Codeine): Withdrawal syndrome (sweating, tremors, nausea)
- Steroids (Prednisolone, Hydrocortisone): Adrenal insufficiency (if stopped suddenly)
- Clonidine (antihypertensive): Rebound hypertension
6. Failure of Therapy (Failure) ADRs
The drug does not work as expected, often due to resistance or interactions.
Examples:
- Antibiotic resistance (e.g., Rifampin in TB treatment): Ineffectiveness due to bacterial resistance
- Oral contraceptives with enzyme inducers (e.g., Rifampin, Carbamazepine, Phenytoin): Contraceptive failure
- Clopidogrel (antiplatelet) in CYP2C19 poor metabolizers: Reduced effectiveness in preventing strokes
- HIV treatment with NNRTIs (Nevirapine, Efavirenz): Drug resistance, leading to treatment failure
- PPIs (Omeprazole, Pantoprazole) with antifungals (Ketoconazole, Itraconazole): Reduced absorption and antifungal failure
7. Idiosyncratic ADRs
Rare, unpredictable reactions due to genetic differences or unknown mechanisms.
Examples:
- Primaquine (anti-malarial) in G6PD deficiency: Hemolytic anemia
- Clozapine (antipsychotic): Agranulocytosis (severe drop in white blood cells)
- Dapsone (leprosy treatment): Hemolysis in G6PD deficiency
- Abacavir (HIV drug) in HLA-B*5701 positive individuals: Severe hypersensitivity reaction
- Isoniazid (TB drug) in slow acetylators: Peripheral neuropathy
Adverse Drug Reaction Classification
ADRs are also categorized based on their cause and nature, which is the Rawlins and Thompson Classification. The two main types of ADRs are:
1. Type A (Augmented) – Predictable & Dose-Related
- These occur due to exaggeration of a drug’s normal effects.
- Usually dose-dependent and predictable.
Examples:
- Low blood pressure (hypotension) from anti-hypertensive drugs.
- Bleeding from excessive anticoagulants (like aspirin).
2. Type B (Bizarre) – Unpredictable & Rare
- Occurs due to individual sensitivity to the drug.
- Not dose-dependent.
Examples:
- Anaphylaxis from penicillin.
- Stevens-Johnson Syndrome from certain antibiotics.
Other types of Adverse Drug Reactions include the following:
Besides Type A and B, ADRs are also classified as the following:
- Type C (Chronic Use) – Due to prolonged use (e.g., kidney damage from painkillers).
- Type D (Delayed Reaction) – Appears after a long time (e.g., cancer due to chemotherapy).
- Type E (End of Use Reaction) – Occurs after drug withdrawal (e.g., seizures after stopping anti-epileptics).
- Type F (Failure of Therapy): Drug does not work as expected (due to resistance, interactions, or poor metabolism). Such as antibiotic resistance (e.g., Rifampin in TB), oral contraceptive failure with enzyme inducers and/or clopidogrel ineffectiveness in CYP2C19 poor metabolizers
- Type G (Genetic/Idiosyncratic ADRs): Rare, unpredictable reactions due to genetic differences. Hemolytic anemia in G6PD deficiency, agranulocytosis or hypersensitivity in HLA-B*5701 carriers.
Difference Between Adverse Event and Adverse Drug Reaction
Many people confuse adverse events (AEs) and adverse drug reactions (ADRs). But they are not the same!
| Features | Adverse Drug Reaction (ADR) | Adverse Event (AE) |
| Definition | Harmful reaction caused by a drug at the normal dose. | Any negative medical occurrence after taking a drug, but not necessarily caused by it. |
| Causality | Directly linked to the drug. | May or may not be linked to the drug. |
| Predictability | Can be predictable (Type A) or unpredictable (Type B). | Can happen randomly. |
| Example | Liver damage from paracetamol overdose. | Fainting after taking medicine (could be due to other causes). |
Not every negative reaction after taking a drug is an ADR. If the cause is uncertain, it’s labeled as an adverse event.
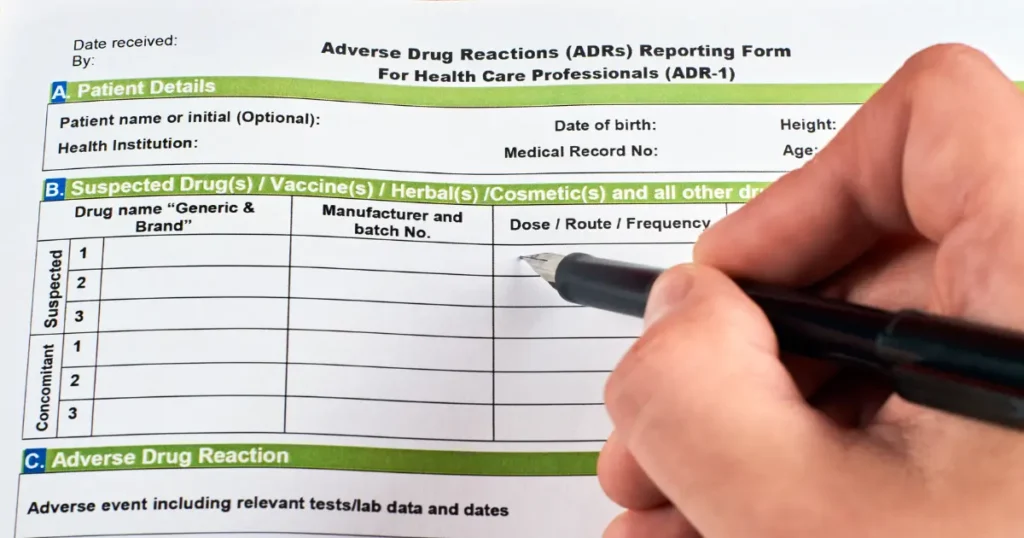
How to Report an Adverse Drug Reaction (ADR)?
Reporting Adverse Drug Reactions (ADRs) is crucial for patient safety, drug monitoring, and improving healthcare outcomes. It helps regulatory authorities assess drug safety and take necessary actions.
Step-by-Step guide to reporting an ADR
1. Identify the ADR
- Check if the reaction is unexpected or severe.
- Determine if the reaction is likely related to the drug (rule out other causes).
- Document the symptoms, onset time, and progression.
2. Collect necessary information
A complete ADR report should include:
- Patient details: Age, gender, weight, medical history, allergies.
- Drug details: Name (brand and generic), dose, route of administration, frequency, and duration of use.
- ADR description: Symptoms, onset time, severity, lab tests, and outcome.
- Concomitant medications: Other drugs the patient is taking (to check for interactions).
- Dechallenge and rechallenge information: Did the symptoms resolve after stopping the drug? Did they reappear after restarting it?
3. Report to the appropriate authority
ADR reporting can be done through:
A. National pharmacovigilance programs
- India: PvPI (Pharmacovigilance Programme of India) – Report via the SUSPECT ADR form or ADR PvPI Mobile App, National Coordinating Centre (NCC-PvPI), Adverse Drug Reaction Monitoring Centres (AMCs) and Online through the PvPI website.
- USA: FDA’s MedWatch (via online form, mail, or phone).
- UK: MHRA’s Yellow Card Scheme.
- EU: European Medicines Agency (EMA).
- WHO: VigiBase (global ADR database maintained by Uppsala Monitoring Centre).
B. Hospital pharmacovigilance centers
- Many hospitals have a pharmacovigilance cell where doctors, nurses, or pharmacists can report ADRs.
C. Pharmaceutical companies
- ADRs can be reported directly to the drug manufacturer, which is required to forward them to regulatory agencies.
D. Online or mobile reporting
- Many regulatory bodies provide web-based portals or mobile apps for easy ADR reporting (e.g., FDA MedWatch, PvPI App, MHRA Yellow Card app).
4. Follow up and monitor
- Keep track of the reported ADR and provide additional details if required.
- Monitor if regulatory agencies issue safety alerts or drug warnings based on reported ADRs.
Here is a short video on: what is Adverse Drug Reaction
Why Report ADRs?
- Improves patient safety.
- Helps identify new drug risks.
- Prevents future ADRs and improves drug monitoring.
- Contributes to global pharmacovigilance efforts.
Who Can Report Adverse Drug Reactions (ADRs)?
Anyone can report an Adverse Drug Reaction (ADR). Reporting is not limited to healthcare professionals—patients and caregivers can also contribute to drug safety monitoring.
1. Healthcare professionals
These professionals play a key role in identifying, documenting, and reporting ADRs:
- Doctors (Physicians, General Practitioners, Specialists)
- Pharmacists (Hospital, Community, Clinical Pharmacists)
- Nurses (Hospital, Clinical, Home Care)
- Dentists (For drug-related oral reactions)
- Medical Students & Interns
- Healthcare Assistants & Paramedics
Why should they report?
- They have direct access to patient medical records.
- They can identify patterns and assess causality.
- Their reports contribute to pharmacovigilance programs.
2. Patients & Caregivers
Patients and their families can also report ADRs.
- Patients experiencing side effects
- Parents or guardians (for children’s reactions)
- Caregivers (for elderly or disabled patients)
Why should they report?
- Some ADRs go unnoticed in clinical settings.
- Patients know their symptoms better than anyone else.
- Direct reports provide valuable real-world data.
In many countries, mobile apps and online portals allow patients to report ADRs easily.
3. Pharmaceutical Companies
- Drug Manufacturers are legally required to collect and report ADRs to regulatory authorities.
- They conduct post-marketing surveillance and monitor adverse effects.
- They are responsible for updating safety labels and issuing warnings.
Why should they report?
- To ensure regulatory compliance.
- To prevent lawsuits and maintain public trust.
- To conduct risk-benefit assessments for drugs.
4. Regulatory & Research Bodies
- Pharmacovigilance Centres (e.g., PvPI in India, MHRA in the UK, FDA in the US)
- Clinical Trial Researchers (For experimental drug reactions)
- Ethics Committees (Monitoring clinical research safety)
Why should they report?
- To detect rare and long-term ADRs.
- To create drug safety alerts and warnings.
- To improve global drug monitoring systems.
On A Final Note…
Adverse Drug Reactions are not just side effects—they can be unpredictable and life-threatening. By reporting ADRs, we can contribute to drug safety and better patient care. If you’re interested in learning more about ADRs, drug safety, and pharmacovigilance, the Learning Labb Research Institute (LLRI) offers specialized courses to help you build expertise in this field.
At LLRI, our courses in Medical Coding, Clinical Research, and Pharmacovigilance teach professionals how to report, monitor, and prevent ADRs effectively, ensuring patient safety in real-world healthcare settings.
Explore LLRI’s courses today and take the first step towards a career in drug safety and clinical research!

